For patients with psychiatric disorders, a bi-directional relationship between inflammation and mood exists. Here, inflammation negatively influences mood, and stress and depression trigger and amplify inflammation. Interrupting this relationship at each point assists patients to improve their mood-based symptoms.
Inflammation Influencing Mood
Multiple meta-analyses have demonstrated increased levels of pro-inflammatory cytokines/markers which are cellular messengers, and C-reactive protein (CRP) in patients with major depressive disorder (MDD) compared to controls.
These elevated cytokines impact mood via:
• Altering the production, metabolism and transport of mood-related neurotransmitters such as dopamine and serotonin
• Impairing neuronal growth and survival, due to the oxidative stress created by inflammatory cytokines
• Dysregulating glutamate levels, leading to excessive excitotoxicity within the brain. This results in reductions in brain-derived neurotrophic factor (BDNF), required to support neuronal health, neuroplasticity, and neurogenesis. Cumulatively, these inflammatory effects lead to the alterations in mood and cognition that present as depressive symptoms.
Mood Influencing Inflammation
Stress and mood disorders can also trigger inflammation. Mechanisms of this include:
• Exposure to early life stressors affects glucocorticoid sensitivity, rendering the immune system less sensitive to normally immunosuppressive cortisol. This change leads to increased rates of inflammatory, metabolic and depressive conditions in later life
• Psychological stressors induce the production of alarmins, molecules that bind to toll-like receptor 4, which triggers release of other pro-inflammatory cytokines.
• Stress triggers a cytokine driven increase in the enzymatic breakdown of tryptophan. This then further promotes depression due to the reduced tryptophan available for serotonin synthesis.
• Psychological stressors are also capable of increasing blood brain barrier (BBB) permeability, allowing the passage of peripheral inflammatory cytokines to enter brain tissue and impact mood.
Modulating Mood and Interrupting Inflammation
Due to the above mechanisms, supporting depression requires an approach that encompasses stress, mood, cognition, and inflammation. The below interventions can be considered:
- Quality fatty acids – EPA and DHA – both of which show benefits in reducing neuro-inflammation and improving mood disorders. However, like with all supplements, not all EFAs are equal. Always consult a qualified Naturopath for high grade products.
- Vitamin D – Optimal levels of vitamin D are required to influence mood-related factors such as neuronal growth and differentiation, monoamine synthesis, and immune modulation. Correspondingly, correcting vitamin D levels via supplementation may improve depression and other symptoms. Only supplement when your levels are low – so check with your health professional before taking any supplements.
- Using apoptogenic herbs which may improve issues with mental alertness, cognition and memory that often accompany depression. Stress can trigger brain changes (e.g. reducing BDNF and increasing neuronal death and neuro-inflammation) that exacerbate depression and its related brain fog. This is why herbs and nutrients that support stress also support mental focus, concentration and memory, are highly indicated.
Whilst evidence highlights this bi-directional relationship that exists between depression and inflammation, there are a myriad of interventions available to address this dynamic from both multiple angles. Reducing inflammatory load whilst also supporting stress, mood and cognition provides a sound foundation for improved mental health.
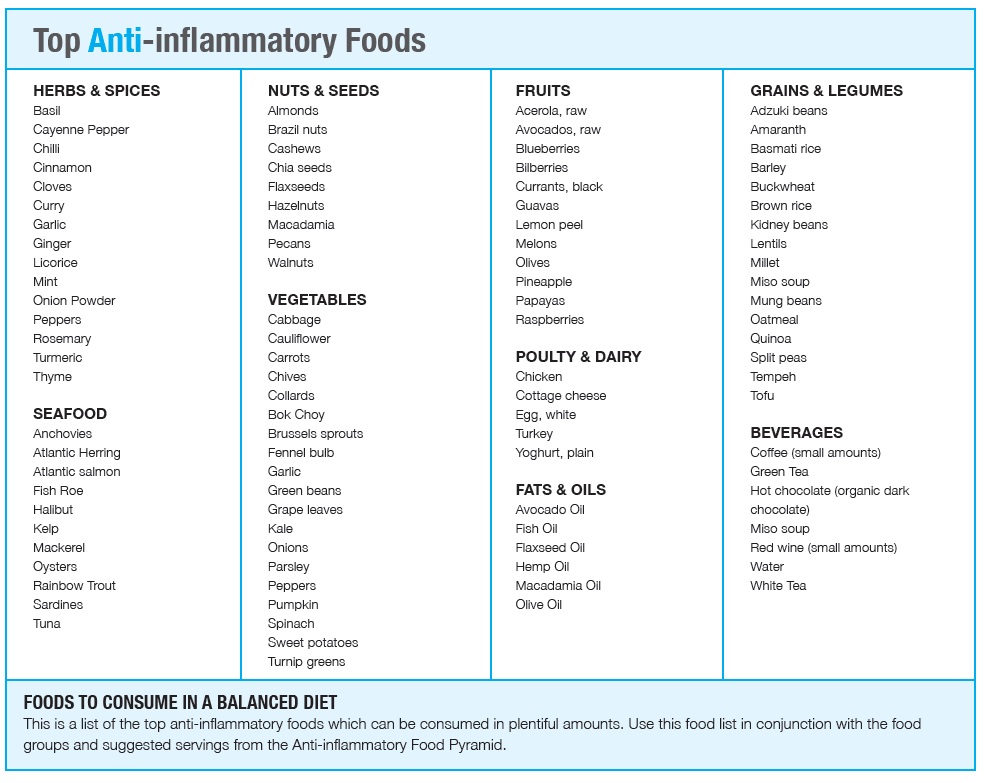
Here’s a list of pro-inflammatory foods to avoid/limit and inflammation-reducing foods to increase in your daily diet.