The following article by Dr Mercola has been reproduced here to maintain access to what is highly relevant and important information for anyone struggling to lose weight, especially those following keto-diets without great success.
STORY AT-A-GLANCE
- Some in the keto and carnivore space argue that eating fats and carbs together will result in weight gain because of the Randle cycle, which serves as a switch that only allows your body to burn either fats or glucose, one at a time, not both together
- The Randle cycle refers to an antagonism between glucose and fats as fuel, which explains why you can become insulin resistant when you avoid carbohydrates
- If you’re in chronic ketosis, your tissues decrease their insulin sensitivity, which can lead to or contribute to insulin resistance
- A low-carb diet is best implemented as a temporary strategy to restore metabolic flexibility. Once metabolic flexibility is regained, adding more carbs back in will help to lower cortisol, which is highly inflammatory
- A narrow time-restricted eating (TRE) window is also counterproductive once you’ve regained metabolic flexibility, as extended fasting also raises cortisol
https://www.bitchute.com/video/uV2Ye2nWciXZ/
Many appreciate my openness to integrating new information into my personal health approach and what I teach. I am a perpetual learner and seek to constantly evolve my approach, so it is aligned with biological truth, even if I have to admit I was mistaken.
Along those lines, I only learned most of the information in this article earlier this year, and it has had a dramatic impact on how I view burning food for energy. This approach is dramatically different than I previously understood and recommended, which was focused on high-fat and low-carb consumption.
You might recall for the last few years I have warned that chronic low-carb eating is not a good idea, and that you need to cycle in and out of low carb. This was a great move in the right direction, but what I have recently learned is that it was not enough and that most people would benefit from far higher amounts of carbs.
When I first started keto, I was below 50 grams of carbs a day for about a year and then for the next five years increased to about 100 grams per day. For the past few months, I have increased that to 425 grams of carbs per day, mostly in the form of ripe fruit.
I have noticed dramatic beneficial changes in my blood work that I won’t go into now but will dive deep into in future articles. I will reveal that increasing my carbs by 400% resulted in a highly counterintuitive, 10% decrease in my fasting blood sugar, and that I also lost 10 pounds despite increasing the number of calories I was consuming — precisely the opposite of what most “experts” would predict.
This doesn’t mean you should stop what you are currently doing and switch, but if you have been struggling with keto and are unable to lose weight, it is likely that a high-fat diet is slowing down your metabolic rate, increasing your cortisol levels and contributing to an inability to achieve your ideal body weight.
My strong recommendation would be to not dismiss this concept as well-intentioned but seriously misguided nonsense, but to take the time needed to understand the solid science behind it.
The reason I switched to the higher carb, low-fat diet was due to learning the late Ray Peat’s work through his student Georgi Dinkov. Peat was a biologist and thyroid expert; Dinkov is a biohack expert. Since the beginning of the year I have been watching Georgi’s videos on YouTube for about two to three hours a day.
He has a thick Bulgarian accent and talks fast so you need to listen at 1X, although I typically watch his videos at least two to five times as it seems every time I relisten to them I learn something new or understand what he has to say in a new way.
Here is a chronologically sorted link to most of his past interviews.1 And wouldn’t you know it, he has not been censored by the globalists, so hundreds of hours are available for free on YouTube and it won’t cost you anything but your time to review.
However, please know that everyone is different and has a unique biochemistry, so your dietary program would have to be customized and fine-tuned for you. Many of the principles are universal and can be widely adopted, though, so If properly done I am convinced that most will notice profound improvement in their metabolic rate, mitochondrial function and energy levels, along with a reduction in inflammation.
Why I Changed My Mind About Low-Carb Diets
One of the foundational concepts of health that I’ve had to radically revise my thinking on, based on Peat’s and Dinkov’s work, is the idea that eating a low-carb diet long-term is the best way to optimize your metabolic and mitochondrial health.
I now realize that this was misguided, and the reason for that has to do with the fact that your body requires glucose, and if you aren’t eating it you will go into a hypoglycemic coma and die. Obviously, your body has safeguards to prevent that, and the major one is the hormone cortisol.
In medical school, we learned that cortisol is a glucocorticoid. Gluco means glucose (sugar) and cortico means it comes from the adrenal cortex. It’s also another word for steroid. We were told that cortisol is responsible for maintaining glucose homeostasis, but led to believe its primary purpose was for inflammation.
Well, that is just not true. While cortisol certainly contributes to glucose balance, its primary purpose is to raise your blood sugar when it is too low and you don’t have enough glycogen reserves in your liver.
How Does Cortisol Work?
But just how does cortisol increase your blood sugar? It does it by breaking down your muscles, bones and brain. It sacrifices your lean muscle mass to release amino acids that your liver converts to glucose in a process called gluconeogenesis.
So, ultimately, cortisol also is going to increase inflammation and impair your immune function. And it increases food cravings. So, you do not want your cortisol to be elevated. For a long time, I was a proponent of a low-carb diet, but now I realize that chronic low-carb is not a good idea.
As a fuel, glucose is vastly superior to fat, and this was something I simply got wrong. The same thing goes for fasting. Both low-carb and fasting are great interventions in the short-term for those who are overweight and metabolically inflexible.
However, once you’ve regained your metabolic flexibility, it is important to revise your strategy and add healthy carbs back in, or these strategies will backfire and lead to decreased metabolic health, compromised mitochondrial function and impaired metabolism.
Cortisol happens to be the primary aging hormone. If it is chronically elevated, you simply will die prematurely as it is highly catabolic, meaning it will break down your body tissues. To stay healthy as you age you need to be anabolic and build healthy tissues like muscle and mitochondria.
Elevated cortisol will seriously impair those efforts. So, it is clear that you need to be doing everything you can to keep your cortisol levels and chronic inflammation low.
The Paradox of Simple Versus Complex Carbs
Since I recorded the video above, it has become clear to me why there is a problem with the seemingly paradoxical conclusion that simple carbs are better than complex carbs for most people. I did not understand this when I recorded the video.
I have since determined that this is a result of most people eating large amounts of metabolic poisons like linoleic acid (LA) their entire life, in addition to regular estrogen exposure in the form of plastics which are xenoestrogens. As a result of these exposures, they have dramatically altered the composition of their microbiomes.
This occurs because these metabolic poisons result in a decrease in cellular energy production in the mitochondria, which then decreases carbon dioxide production in the intestine. The relatively lower concentration of carbon dioxide in the large intestine promotes the growth of pathogenic disease-causing bacteria known as facultative anaerobes.
These specific bacteria have high amounts of lipopolysaccharide (LPS) embedded in their cell membranes. When they are provided with food in the form of complex carbohydrates, they serve as fertilizer to accelerate their growth, so they multiply and eventually die.
When they die, this LPS, otherwise known as endotoxin, is released, and that is another potent metabolic poison that will radically decrease your mitochondria’s ability to create cellular energy, thus contributing to a vicious downhill cycle.
This sets up the seemingly paradoxical scenario where healthy food such as complex carbohydrates can make your health worse, because they are increasing the concentration of endotoxin in your body, which in high concentrations can result in septic shock that kills you.
The solution is to improve your health by improving your mitochondrial function and their ability to create sufficient cellular energy, which will subsequently restore the balance of healthy bacteria in your gut. When this is achieved, then complex carbohydrates transition to becoming very healthy.
But until your mitochondria produce adequate energy, complex carbs frequently contribute to worsening your health through the production of endotoxin. So it’s wise to carefully navigate with the introduction of complex carbs if you have been exposed to metabolic poisons for most of your life.
I believe the most prudent strategy is to listen and trust your body. If you have any problems eating complex carbs that result in bowel symptoms, then it would be wise to consider restricting your carbs to very simple carbohydrates such as fruit juice, which is the easiest carbohydrate to digest.
Once that is tolerated then you can go to healthy whole fruits. Once that is tolerated then you can progress to including other more forms of more complex carbohydrates until you are feeling that you can tolerate those.
Important Cautions Before You Increase Carbs
It would be a major mistake to increase your carb intake if you are still on a high-fat diet. I did this experiment in the mid-‘80s after I read the book by Harvey and Marilyn Diamond called “Fit for Life.”
They suggested having fruit only for breakfast – which I tried. Then I did my lab work and found my fasting triglycerides and lipoprotein profiles had exploded for the worse. I prematurely concluded that a high fruit diet was nonsense and remained relatively low-carb for nearly four decades.
This was until I encountered Ray Peat’s work and reevaluated my initial impression. I now understand that I was missing important parts of the strategy. And now I eat 3 to 4 pounds of watermelon every morning at 5:30 as my first meal, followed by three eggs and 8 ounces of white rice and 2 ounces of maple syrup one to two hours later.
That sounds like a lot of carbs, and it is. I have additional fruits later in the day and now my carb intake is about 425 grams a day. You might wonder what has happened to my weight and blood sugar with all these extra carbs.
Well, I thought my weight was good at 192 as I increased my muscle mass, but it has decreased by 10 pounds to 182 with no change in muscle mass. My fasting blood sugar has dropped 10 points and, so far, it seems to be working for me.
The Vital Metabolic Switch You Need to Understand
This is one of the most important principles in food science that I had never learned or understood until recently. My strong guess is that this is also true for most natural medicine clinicians. That is why I created the figure below to help you visualize it, so you can better understand this vital concept.
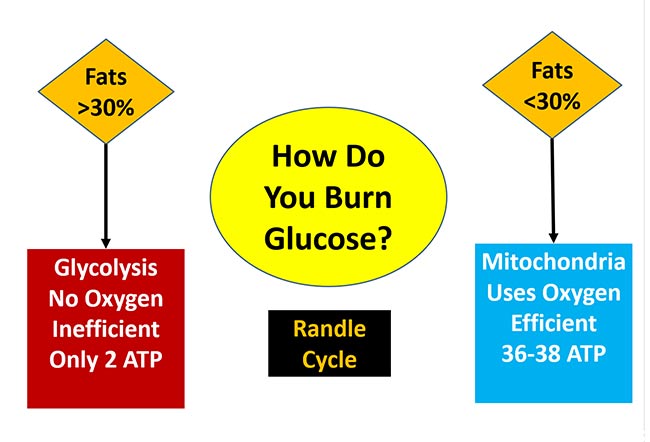
Low-carb diets have helped at least tens of millions of people improve their health for a very good reason, and that is there is a stealth switch that controls what fuel your mitochondria can burn. They can only burn one fuel at a time, either fat or glucose.
The switch has been given the name the Randle cycle, but it is more helpful to visualize it as a railroad switch that changes the tracks of the train. The train can only travel down one track; not both. This is because only one type of fuel can be burned at a time.
The best-case scenario is you metabolize, or burn, glucose in your mitochondria without any reductive stress (a term I will explain in my upcoming interview with Georgi Dinkov). When you do this, you will only generate 0.1% reactive oxygen species (ROS).
Not only does this route generate less ROS, but it also is incredibly efficient at energy production by creating 36 to 38 Adenosine triphosphates (ATP) for every molecule of glucose that is metabolized. It will also generate metabolic water and carbon dioxide, which are also important for your health.
For this to occur, as indicated in the figure above, you will need to consume less than 30% of your calories as fat. When you consume significantly more than that amount, the switch changes to burn fat in your mitochondria and you will not be able to burn glucose until your fat decreases to less than 30% of calories.
Since glucose is unable to be shuttled into the mitochondria to burn, it winds up backing up into your bloodstream, raising your blood sugar. This is a major contributor to diabetes. What little glucose is burned for fuel is done by using glycolysis, which is a primitive pathway that bacteria and cancer cells use.
It is great that we have this pathway, as you absolutely need it for quick fuel when you are activating your type II muscle fibers. But if this is the primary way you burn glucose, you are in a catastrophic metabolic state as you are creating loads of lactic acid as a waste product instead of healthy CO2. And, you are only generating two ATP for every molecule of glucose, which is 95% less energy.
Lactic acid increases reductive stress, which causes reverse electron flow in the mitochondria and causes reductive stress, which increases the ROS to 3% to 4%, which is 30 to 40 times more than when glucose is burned efficiently in the mitochondria. You likely don’t yet understand reductive stress, the opposite of oxidative stress, but I will be doing an interview with Georgi on this and will be posting it later this month.
Why Lactic Acid and CO2 Are so Important
Remember, when you are burning glucose efficiently in your mitochondria, the glucose is converted not only to 36 to 28 ATP, but when the electrons from the glucose are ultimately handed off to oxygen, metabolic water (deuterium free) is made and, very importantly, carbon dioxide.
This is vital to understand as carbon dioxide is a potent stimulator of mitochondrial biogenesis which will increase the number of mitochondria that you have so you can make even more energy.
Conversely, when you are burning glucose far less efficiently in glycolysis you are only generating two ATPs, and rather than creating life-sustaining carbon dioxide, you are generating life-damaging lactic acid, which will degrade your mitochondria and make them die sooner.
In this second video, Paul Saladino interviews Dinkov about the Randle cycle. Dinkov comments:
“The first accusation against you, that whole milk will somehow make you fat because of the Randle cycle [is] misguided because if you look at the label, whole fat milk has like 5 grams of fat per serving but 12 grams of carbs, so you’re actually [getting] more carbs.
But let’s talk about meat. Most meats … are actually not that high in fat, and a lot of the fat in them is actually short chain fatty acids, which are not subject to the Randle cycle because they get transported into the cells through a known L-carnate-independent mechanism.
They metabolize similarly to sugar, and they don’t seem to be triggering the same sort of Randle cycle effect. Now, what drives the Randle cycle effect? When you’re oxidizing primarily fats … the master conductor redox modulator — which is the NAD to the NADH ratio, specifically the intra-mitochondrial one — drops. (This simply means the more NAD+ the better).
Basically, the NAD to the NADH ratio — which signals how oxidized versus how reduced you are, metabolically — [is] the primary regulator of whether the pyruvate dehydrogenase (PDH) will accept pyruvate and convert it into acetyl-CoA and then continue with the Krebs cycle in the electron transport chain, or not.
(Pyruvate is the three-carbon molecule breakdown product of glucose. PDH is the enzyme that converts it to acetyl-CoA which allows it to enter the mitochondria and be burned efficiently. If PDH is inhibited, it will force your body to use fat).
In other words, a high ratio of NAD to NADH (meaning high NAD+) when you’re very oxidized favors the activity of pyruvate dehydrogenase, so you will not be accumulating pyruvate [and] you will not be generating lactate.
But if you’re eating a lot of fat, the NAD to the NADH ratio drops, and then the buildup starts to happen. Pyruvate accumulates, lactic [acid] accumulates. [This means] the Krebs cycle is working because it’s accepting acetyl-CoA from the beta oxidation. That’s how the fatty acids get oxidized.
So, that’s the gist of the Randle cycle … If you’re providing a lot of glucose, in theory you should be able to out-compete the free fatty acids and oxidize more glucose versus fat, but that all depends on how much glucose can get into the cell.
And, unfortunately, when you’re eating these high-fat diets, when you have higher lipolysis, the actual uptake of glucose into the cell is already largely blocked …
Free fatty acids not only block the metabolism of glucose, they also block the uptake of glucose into the cell. So, they prevent the positive effects that the glucose would have had, in terms of competing with the free fatty acids …
Basically, too much fat blocks your uptake and utilization of glucose, and whatever glucose is taken up, you largely convert to nonbeneficial byproducts such as lactic acid …”
So, to summarize Dinkov’s rather complex exposition on the Randle cycle’s effects: a) fats can make you fat directly; and b) fats limit your ability to metabolize glucose. This is due to the Randle cycle’s preference to fat metabolism when more than 35% of your calories come from fats. And, even if you metabolize small amounts of glucose, your body will favor the conversion of glucose into fat versus ATP, water and carbon dioxide.
This is because the enzyme PDH, which converts the glucose metabolite pyruvate, is inhibited by high fat concentrations, and won’t convert pyruvate to acetyl-CoA to be burned in the mitochondria. Instead, because PDH is inhibited, the pyruvate is metabolized into lactate. This entire process is antimetabolic and slows down your metabolism, increases your ability to gain weight, and lowers your ability to generate cellular energy.
So, when more than 30% to 35% of your calories are coming from fat, you are forcing your cells to burn fat and put glucose on the back burner, instead of being metabolized like it should be.
Simple Strategies You Can Implement to Help Your Metabolism
Clearly, the most important strategy to help your metabolism is to avoid eating linoleic acid at all costs. It is impossible to avoid as it is in nearly every food, but you want to keep your levels below 2% of your daily calories. This means avoiding ALL processed foods and typically most restaurants.
A powerful strategy that nearly everyone should do is to make sure that you are taking a high-quality vitamin E supplement once a day. Why? Because most everyone has 20 to 30 times more LA in their body than optimal. Not only will vitamin E impair the release of it from fat cells, but once released it will help protect the LA from converting into dangerous oxidized linoleic acid metabolites (OXLAMs).
Most vitamin E supplements should be avoided, so how do you identify a high-quality vitamin E supplement? It should have most of the vitamin E isomer as alpha tocopherol, typically about 150 units. It should also have the other tocopherol isomers: alpha, beta and gamma, but at far lower doses.
Additionally, it should have alpha, beta and gamma tocotrienols. Finally, it should only have the “D” isomer. Avoid all vitamin E supplements that are “DL,” which are 50% of the wrong isomer.
It would be very wise to make sure you have enough NAD+ as it will also inhibit the release of LA from your fat cells. If you haven’t read and viewed by interview with molecular biologist Nichola Conlon on this topic, you can read it on my Substack. Sadly, NAD+ decreases dramatically as you age, which leads to nearly a 1-to-1 reduction in ATP, your cellular energy currency.
Fortunately, this can be inexpensively addressed by taking 50 mg of niacinamide three times a day. More is not better, so avoid 500 mg tablets as they will impair your longevity proteins. Typically, one sixty-fourth of a teaspoon of niacinamide powder is about 50 mg.
Finally, aspirin can be a very useful way to inhibit LA lipolysis. Aspirin is a very interesting approach and I go into far more details in my recent article on it.
Why Long-Term Low-Carb Diets Can Backfire
I previously touched on the Randle cycle in “How the Wrong Dietary Fat Can Wreck Your Health,” which also featured an interview with Dinkov. In that interview, Dinkov cleared up several areas of confusion, including the following:
•Low-carb dieting is a great short-term intervention for people who are overweight and insulin resistant. Lowering carbs will help reset your metabolism and recover your metabolic flexibility. However, in the long-term you will likely run into trouble — especially if you’re also doing a lot of endurance training.
One of the reasons for this is because when you’re in a low-carb state, lipolysis is elevated, which releases inflammatory polyunsaturated fatty acids (PUFAs) such as LA from your cells that are then into dangerous OXLAMs (oxidative linoleic acid metabolites) that will damage your tissues.
PUFAs such as LA are not digested. Instead, they’re stored.2 Most of the body fat in obese individuals is composed of PUFAs, not saturated fat. Saturated dietary fat is mostly burned (oxidized) and used up. So, most people have large stores of LA, and these stores need to be lowered to safe levels of 1% to 2% LA.
•Extended fasting and using an excessively narrow time-restricted eating (TRE) window can also backfire once you’re metabolically flexible, as it too helps push LA out of your cells.3,4,5,6,7,8,9,10 An extreme example of TRE is the one meal a day (OMAD) protocol, where you’re fasting 22 hours or more each day. Dinkov believes this is too extreme for most people.
The half-life of PUFAs such as LA, which get embedded and integrated into your cell membranes, is about 680 days. This means that ridding your body of LA will take approximately seven years, provided you don’t load more in. And you really do want to get rid of this fat, as it’s highly inflammatory and prevents your mitochondria and cellular machinery from operating properly. But you need to do it slowly and methodically.
Exercise and fasting will help drive the LA out, but you need to be really careful if you have a lot of LA storage. You want to avoid excessive lipolysis — any situation where you’ve run out of glycogen, which can easily happen when you’re not eating for long periods, when you’re on a chronic low-carb diet, and/or when you’re engaging in intense exercise, especially if you exercise in a fasted state.
•Chronic long-term, low-carb, and chronic extended fasting also result in elevated cortisol, which is highly inflammatory and promotes the storage of fat. Elevated cortisol is also highly catabolic and will cause you to lose lean muscle mass so your liver can make glucose. For these reasons, low-carb diets and fasting are best implemented as temporary strategies to restore metabolic flexibility.
How to Safely Reduce LA Stores Without Self-Sabotaging
With all of that in mind, how can you safely reduce your LA stores without self-sabotaging? Extensive fasting will, in this instance, backfire, as will overtaxing yourself with heavy exercise. You’ll need to accept that achieving optimal health is a marathon, not a sprint, and that it’s going to take years to purge your LA stores. Dinkov suggests the following strategy:
- Build muscle and maximize lean muscle mass
- Avoid fasting for longer than 16 hours
- Avoid all processed foods, restaurant foods, condiments and animal foods raised on grains, such as chicken and pork, as all of these are high in LA
- Eat a diet with about 15% protein, restricting fats to below 35% with the remainder consisting of carbs in the form of ripe fruits and some vegetables and well-cooked low-oxalate starches. Be careful to avoid all processed sugars as they typically are loaded with high fructose corn syrup that will increase endotoxin in your gut
So, to recap, temporarily implementing a six- to eight-hour time restricted eating window, or even longer eating restrictions and fasts, is appropriate for anyone who is insulin resistant and metabolically inflexible — and that’s about 95% of the population.
However, once you lose your insulin resistance and become metabolically flexible — which typically takes a few weeks — you’ll want to increase your eating window to eight to 12 hours to avoid elevating your cortisol, as cortisol promotes chronic inflammation that can lead to tissue damage, and promotes the storage of fat.
How does TRE and extended fasting raise cortisol, you ask? It is important to understand that cortisol is a powerful hormone whose primary purpose is to shred your lean muscle mass and bones to obtain amino acids for your liver so it can produce glucose. This is cortisol’s primary role. If your blood sugar gets too low, you will go into a hypoglycemic coma and die. Your brain requires sugar and if it doesn’t get it, it is game over.
Usually, it takes a few weeks and occasionally longer, for you to recover your metabolic flexibility. During those first three to six months, stick to a six- to eight-hour eating window. Once you’re metabolically healthy, avoid eating windows under eight hours. I’ve now shifted to a schedule where I always have an eating window of more than eight hours a day and closer to 12, in the summer when there is plenty of daylight.
Interestingly a recent study showed that a lower fat, higher carb approach lowers the risk of death by 30%, while with the converse a high-fat, low-carb diet increases the risk of death by 30%.11,12 So, it’s your choice for sure, but I am convinced that having more healthy carbs than fat is a great choice to improve your metabolic health.
Sources:
- 1 YouTube Georgi Dinkov
- 2 Haidut.me October 22, 2019 (Archived)
- 3 Haidut.me February 16, 2021 (Archived)
- 4 Haidut.me September 27, 2022 (Archived)
- 5 Haidut.me March 4, 2021 (Archived)
- 6 Haidut.me December 10, 2021 (Archived)
- 7 Haidut.me June 21, 2022 (Archived)
- 8 Haidut.me November 17, 2020 (Archived)
- 9 Haidut.me December 21, 2021 (Archived)
- 10 Haidut.me September 30, 2020 (Archived)
- 11 J Intern Med. 2023 May 3. Low-carbohydrate diets, low-fat diets, and mortality in middle-aged and older people: A prospective cohort study
- 12 Haidut.me May 9, 2023 (Archived)
