Inflammation in response to physical trauma often includes heat, swelling and pain – all intended to immobilise the affected area to enable healing. Once the tissue has healed, inflammation has also cleared. However, there is a serious form of systemic inflammation that becomes chronic and has been attributed to many diseases. It is this low-grade chronic inflammation that often goes unnoticed until there is a major health issue.
Systemic, chronic inflammation underlies many diseases
Inflammation is a normal and protective biological mechanism necessary for fighting pathogen infiltration and managing physical trauma. In these acute scenarios, inflammation is only present for the time that it takes to resolve the infection or heal the trauma, after which, it is resolved.
In contrast, systemic, chronic inflammation (SCI) arises in response to stimuli such as chronic infection, obesity, gut dysbiosis, poor diet, and environmental pollutants, and has long-lasting and pervasive efects.1
SCI driven diseases account for more than 50% of all deaths worldwide, including ischemic heart disease, stroke, cancer, diabetes, chronic kidney disease, non-alcoholic fatty liver disease (NAFLD), autoimmune and neurodegenerative diseases.1
Considering these statistics, SCI can be considered the major driver of modern disease. Thankfully, natural medicine offers powerful agents to combat SCI.
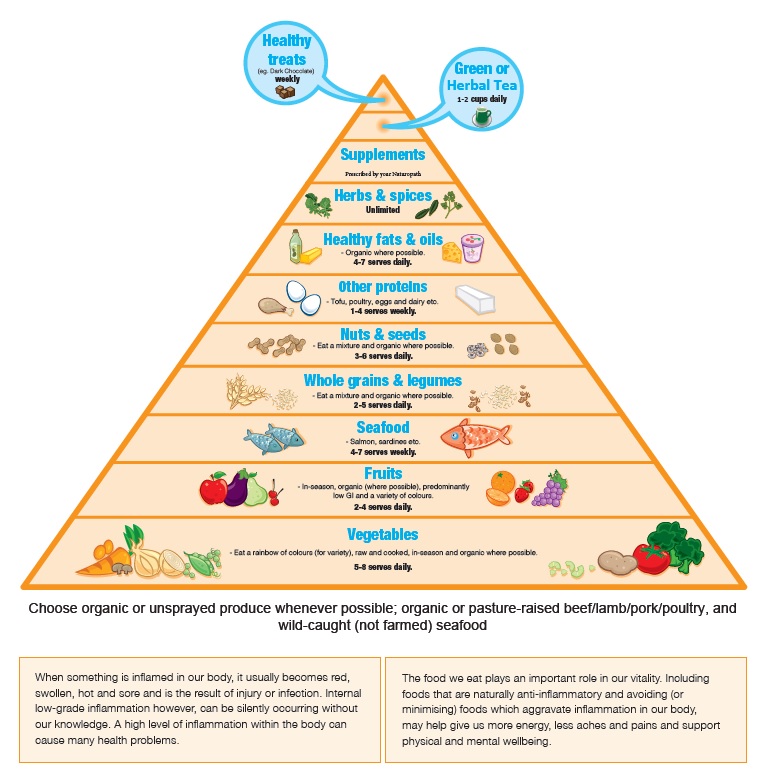
How nutrition can help combat SCI
Low or imbalanced mineral and nutritional status have been identified as major factors influencing onset, intensity and duration of inflammatory conditions.2,3 There is an inverse correlation between higher levels of magnesium and lower levels of the inflammatory marker CRP (serum levels of C-Reactive Protein).4 Magnesium deficiency could be seen as another driver of chronic disease, either initiating or perpetuating the disease process through an enhanced inflammatory response.
An inadequate magnesium intake is common in Australians, particularly in the elderly and teen years.5 For example, over 30% of Australian adults do not consume the estimated average requirement (EAR) for magnesium. Higher numbers were observed (30-70%) for teens aged 14-18 and those over 50.5
In addition, magnesium levels are reduced by the intake of alcohol, salt, carbonated beverages and coffee, as well as from profuse sweating, intense exercise, excessive menstruation, some parasites and many medications.6 As such, magnesium supplementation may be required to establish an adequate mineral status. A meta-analysis of eight studies found that magnesium supplementation (ranging from 340-1500 mg/d) results in a 1.33 mg/dl reduction in CRP.7 When the studies were analysed according to baseline CRP levels, researchers found a more profound impact of -0.295 mg/dl for those with a baseline CRP of ≥ 2mg/dl.7 Magnesium supplementation was also found to significantly reduce TNF-α [Tumor necrosis factor is a cell signalling protein involved in systemic inflammation and is one of the cytokines that make up the acute phase reaction].7 The effects of magnesium supplementation on reducing inflammation may go a long way towards chronic disease prevention.
However, not all forms of minerals are readily absorbed and available for your body to use. One of the better forms of minerals are the citrates as these also help maintain healthy pH levels (acid-alkaline balance).8 Achieving optimal inflammation modulation requires careful balancing and combining of nutrients which is why you should always consult a qualified naturopath and resist the temptation to self-prescribe.

REFERENCES – Article courtesy of BioPractica Nutraceuticals
1 Furman, D., Campisi, J., Verdin, E., Carrera-Bastos, P., Targ, S., Franceschi, C., Ferrucci, L., Gilroy, D. W., Fasano, A., Miller, G. W., Miller, A. H., Mantovani, A., Weyand, C. M., Barzilai, N., Goronzy, J. J., Rando, T. A., Effros, R. B., Lucia, A., Kleinstreuer, N., & Slavich, G. M. (2019). Chronic inflammation in the etiology of disease across the life span. Nature medicine, 25(12), 1822–1832.
2 Nielsen F. H. (2018). Dietary Magnesium and Chronic Disease. Advances in chronic kidney disease, 25(3), 230–235.
3 Nielsen F. H. (2018). Magnesium deficiency and increased inflammation: current perspectives. Journal of inflammation research, 11, 25–34.
4 Song, Y., Ridker, P. M., Manson, J. E., Cook, N. R., Buring, J. E., & Liu, S. (2005). Magnesium intake, C-reactive protein, and the prevalence of metabolic syndrome in middle-aged and older U.S. women. Diabetes care, 28(6), 1438–1444.
5 https://www.abs.gov.au/statistics/health/health-conditions-and-risks/australian-healthsurvey-usual-nutrient-intakes/latest-release#essential-minerals
6 Johnson S. (2001). The multifaceted and widespread pathology of magnesium deficiency. Medical hypotheses, 56(2), 163–170.
7 Mazidi, M., Rezaie, P., & Banach, M. (2018). Effect of magnesium supplements on serum C-reactive protein: a systematic review and meta-analysis. Archives of medical science : AMS, 14(4), 707–716.
8 Walker, A. F., Marakis, G., Christie, S., & Byng, M. (2003). Mg citrate found more bioavailable than other Mg preparations in a randomised, double-blind study. Magnesium research, 16(3), 183–191.
