Comments on The Courier Mail, QWeekend article “A heavy burden”
by Elissa Lawrence, May 2-3, 2015.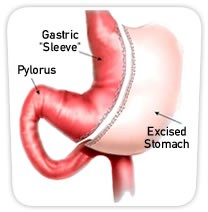
This story related to six members of one Brisbane family who have had weight-loss surgery to help with obesity. The type of surgery undertaken is called a sleeve gastrectomy which involves surgically removing nine-tenths of the stomach. The removal of most of the stomach leaves a sleeve-like tube restricting stomach capacity to about 200ml.
The above diagram shows how much of the stomach is removed. This procedure is permanent.
The stomach is an essential organ
When we eat, the cells of the stomach lining produce secretions to begin the digestive process – most importantly hydrochloric acid for protein breakdown and intrinsic factor to assist with Vitamin B12 absorption. The stomach also churns the food to ensure proper mixing with the digestive juices. By removing the majority of the organ, not only is the volume drastically reduced, but so too is digestive capacity. In addition to a significant reduction in the amount of food that will fit into the remaining stomach sleeve, there is also a significantly reduced ability to absorb nutrients. Weight loss is an obvious result, but so is malnutrition.
The low stomach pH (high level of hydrochloric acid) not only breaks down protein but is also essential for the body’s absorption of calcium, magnesium, iron and zinc. These are essential minerals for bone, heart, blood, nerve and muscle health.
This type of surgery currently costs in the vicinity of $15,000.
The article discusses the family all of whom have always been ‘large’. Only very briefly does it report that they all grew up “with unhealthy food habits” involving lots of “biscuits and cake and desserts.” It goes on to state that following this surgery, “You’ve got to eat properly, you have to exercise, take your vitamins, drink enough water … it’s a mindset change”. The family involved also admit they had to “learn how to eat again, what to eat.”
So the question must surely be asked: why could this mindset change not have led to healthy eating and lifestyle habits including exercise BEFORE 9/10ths of the stomach is removed permanently?
This surgery for a family of four would cost around $60,000. For far less, that family would be able to enlist the support of a qualified nutritionist, cook and exercise therapist to achieve lasting, sustainable weight loss and create long term health. Healthy lifestyle habits would then be passed on to subsequent generations, turning around the obesity epidemic in this family.
Instead, they are upset that the 11 year old son, who currently weighs 90kg, can’t get this surgery until he turns 14 years of age (with his projected weight to reach 140kg by age 15).
The true cost of weight-loss surgery
Whilst this surgery will lead to weight loss – initially – it will also lead to malabsorption issues. Diseases associated with malabsorption of essential nutrients include osteoporosis, cardiovascular disease, fatigue, hormonal imbalances, immune dysregulation, irritable bowel syndrome, depression and other mental health issues. It seems that these consequences of lucrative surgery are largely ignored by the surgeons.
There are some who believe that gastric sleeve surgery should be paid for by the Government. Surely investing a fraction of the cost of this surgery in health education would achieve better results leading to a healthier Australia?
