The following article has been published here with approval of the author BioMedica Nutraceuticals
The interplay between mould exposure and human health is still not fully elucidated. While the induction of allergic immune responses by moulds is generally acknowledged, other direct health effects such as mould illness or toxic mould syndrome, are less understood. However, recent observations and evolving research highlights the potentially significant role of mould/mycotoxin exposure in individuals with pre-existing dysregulation of the immune system, and in those exposed to water damaged buildings.
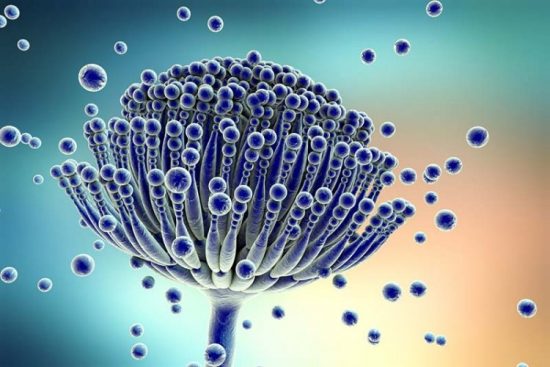
Moulds and mycotoxins
Mould is a type of fungi which is present in both indoor and outdoor environments,1 and is capable of producing a number of metabolites, some of which are harmful to human health. Mycotoxins are diverse toxic secondary metabolites that are naturally produced by a wide range of moulds. Individual mould species can produce many different mycotoxins2 and to date, several hundred mycotoxins have been identified.1 Indoor environmental mycotoxin contamination is recognised as a global problem, especially in developing countries.3
The health effects associated with fungi exposure can be categorised as infections (mycosis), allergic reactions, or toxic effects,4 and usually require exposure to spores via inhalation, ingestion of contaminated foods or skin contact.5 For fungi to infect humans, four criteria must be met: growth at human body temperatures, circumvention or penetration of surface barriers, lysis and absorption of tissue, and resistance to immune defences including elevated body temperatures.6
In the past decade, mycotoxins have attracted considerable attention due to their potential for strong toxicity. Evolving research is highlighting the harmful effects of mycotoxin exposure, including acute poisoning and death,7 irreversible liver damage,7 respiratory impairment,8 gastrointestinal damage,9 and neurotoxic effects.10,11 More recently, toxic mould syndrome and associated biotoxin-related illnesses have been critically discussed as a potential emerging global health crisis.1,12-14
What is mould illness and toxic mould syndrome?
Humans are exposed to multiple fungi, many of which are not harmful to health and rarely cause disease. In healthy humans, invasive fungal disease is rare due to the evolution of sophisticated immune systems which constantly respond to fungal exposure.15 However, there are well known instances where mould and mycotoxins have significantly harmed human health, such as in the cases of black mould and aflatoxins.7
Toxic mould syndrome or mould illness is described as a symptom complex with a wide variety of presentations, such as cognitive impairment, emotional disturbance, respiratory complaints and muscle aches.12,13 Despite the need for more rigorous research in this syndrome, moulds and their mycotoxins have been shown to induce direct hypersensitive reactions and can induce immune dysfunction in immunocompetent individuals.1 There is growing evidence that mycotoxins are of significant concern for individuals with pre-existing dysregulation of immune function, leading to systemic, multi-symptom presentations.

Mould and Chronic Inflammatory Response Syndrome (CIRS)
Chronic mould exposure has been shown to induce inflammation and immune system dysregulation in response to specific mould and mycotoxin challenges ex vivo.16 In addition, there is a small amount of evidence to suggest that the systemic inflammation which results from mycotoxin exposure can lead to structural brain abnormalities due to increased permeability of the blood-brain barrier.17 CIRS has been described as a chronic, multisystem and multi-symptom syndrome that has been attributed to mould exposure, and has been associated with a range of physical and cognitive symptoms, including fatigue, pain, gastrointestinal and sinus issues, and memory difficulties18 (see Figure 2). Unfortunately, this syndrome and the associated chronic symptom complexes remains poorly understood.
The Standing Committee on Health, Aged Care and Sport recently made an enquiry into biotoxin-related illnesses in Australia.18 Throughout the enquiry, the Committee was presented with a range of views and personal accounts regarding CIRS, particularly in its relation to living and working in buildings with significant mould growth or water damage. It was concluded that complex illnesses such as CIRS and other biotoxin-related illnesses remain difficult to diagnose and treat, and their prevalence remains unknown. It was recommended to the Department of Health that future options be considered to improve the diagnosis and treatment of complex illness and unexplained symptoms, in order to help reduce the financial and social burden for patients, and ensure health professionals are provided with adequate support and training.
Mould and sick-building syndrome
The importance of indoor fungal growth in human health continues to become evident, as reports of building-related illnesses rise globally. The interplay of site characteristics, climate, building system, construction materials, building dampness, contaminant sources and activities of occupants, can all affect the quality of indoor air.14 Previous studies have demonstrated that the indoor air of water-damaged buildings contain a complex mixture of fungi, mycotoxins, bacteria, endotoxins, antigens, lipopolysaccharides, and biologically produced volatile compounds, all of which pose a significant health risk to exposed occupants.20,21
Occupants of water-damaged buildings with evidence of microbial amplification often describe a syndrome involving multiple organ systems, commonly referred to as “sick-building syndrome” (SBS).20 SBS manifests as a complex spectrum of symptoms, such as mucus membrane irritation, asthma, neurotoxic effects, gastrointestinal disturbance, skin dryness and sensitivities to odour, similar to other reported biotoxin-related illnesses.
Concerns about human health due to deteriorating indoor environmental quality is steadily increasing, and acknowledging the incidence of SBS symptoms seems straightforward. However, its characterisation and linkage to indoor exposure requires in-depth analysis, and further research is required to examine how environmental processes trigger health symptoms and whether some individuals are more prone to illness as a result.
Mould-affected housing in Australia
In response to the Australian government enquiry into biotoxin-related illness, a recent integrative review of 45 studies aimed prevalence, risk factors and impacts related to mould-affected housing in Australia.22
The most commonly reported relationship was that of indoor mould/mildew/fungi and risk factors or associations with poor housing conditions, socioeconomic circumstance or building characteristics. This was closely followed by the reported prevalence of visual mould/mildew or measured fungi in housing and its relation to perceived or measured health impacts. Unfortunately, there was no available Australian literature found relating to three major risk factors: climate, urbanisation and building maintenance. The highlights were as follows:
- Poor housing conditions from mould, dampness, cold and cracks were reported in twelve of the included studies, with rental properties being the most represented.
- The presence of mould/mildew/fungi-affected dwellings was reported in approximately half of the included studies.
- The majority of the included health studies supported a causal relationship with mould/mildew/fungal indicators and asthma, wheeze, cough and other respiratory symptoms as well as associations with domestic allergic alveolitis and hypersensitivity pneumonitis.
- Seven other studies reported a relationship between allergy, atopy, gastrointestinal symptoms, mood changes, depression and pain, and indoor mould/mildew/fungal indicators.
- Five studies reported a mixed variety of symptoms similar to that of SBS and overlapping environmental illness conditions in relation to indoor mould.
Unfortunately, this review also highlighted the inconsistencies in the available national housing survey data and how mould-affected housing has been studied overtime. Future research into mould-affected housing is critical to support healthier housing, and regulatory housing decisions within Australia, especially since Australia experiences climate vulnerability, extreme weather events and there is a shift towards a greater number of Australians spending more time at home.

Mould-induced immunological effects
Mould-induced hypersensitivity
Mould can cause different hypersensitivity reactions.23 So far, 88 allergens have been isolated from four genera of fungi belonging to the Ascomycota phylum, including Aspergillus and Penicillium species.1 Allergens that have been isolated from mould include enolase, heat shock proteins, cyclophilins, proteases, redoxins and disulphide isomerases.24,25 However, there is currently no evidence that mycotoxins may function as allergens.
Type 1 allergies are characterised by antigen-specific IgEantibodies which are produced shortly after exposure to already sensitised mould agents.26 Although the exact prevalence is unknown, there are many studies which implicate mould as an allergen in allergic asthma.27 Recent studies indicate various indoor and outdoor mould species like A. alternata and A. fumigatus exert strong inflammatory and allergenic properties in asthmatics with mould sensitisation.28 Also, fungal rhinosinusitis, which is a subset of chronic rhinosinusitis with nasal polyps has been classified as a type 1 allergy with elevated levels of mould-specific IgE.29
In addition to type 1 allergies, mould can also induce type 3 and 4 hypersensitivity reactions, known as hypersensitivity pneumonitis.30 Hypersensitivity pneumonitis has been associated with airway exposure to high concentrations of mould spores, especially due to occupational conditions like farmer’s lung, or trombone player’s lung in wind musicians.30-32
Mycotoxins and immune dysregulation
Mycotoxins occurring in food have been associated with immune deficiency, which can result in an increased susceptibility to infection and cancer.7 A recent review article explored the immunotoxic effects of aflatoxin and while the underlying mechanisms related to immunotoxicity are still under investigation, it is suggested that aflatoxin can induce both immunosuppressive and immunostimulatory effects.33 A recent in vivo study showed that aflatoxin M1 suppresses innate and acquired immunity,34 while patulin, another mycotoxin found in several fruits and their products has also been shown to suppress innate immune responses in vitro.35
The immune system plays a central role in mould-host interaction, and immune responses against mould have been shown to be species- and mycotoxin-dependant.36 Trichothecenes, aflatoxin, gliotoxin, ochratoxin, citrinin, ergot alkaloids and patulin, among others have been studied in vivo and in vitro to identify cellular targets and molecular mechanisms of action.37 Recent research has uncovered that mycotoxins can affect different immune cells through the induction of apoptosis and the suppression of specific immune cell function.38
Mycotoxins as secondary metabolites of moulds have been shown to have multiple mode of actions in vivo and in vitro, including impairment of barrier functions, exacerbation of inflammation, alteration of gut microbiota and interference of T cell differentiation (Figure 3).1 In addition, it appears that mycotoxins are systemically bioavailable irrespective of the route of exposure. Mycotoxin exposure via the airways results in systemic bioavailability in vivo39 and oral mycotoxin intake results in chronic inflammation in the lungs,40,41 resulting in multi-organ exposure. This systemic bioavailability may support the ability of mould and mycotoxins to produce systemic, multi-symptom presentations such as CIRS, SBS and toxic mould syndrome.
While the mechanisms of immune dysregulation are still not fully understood, the available research undoubtedly highlights the potential for mycotoxins to elicit effects on immune, gastrointestinal and barrier function, and would suggest the impact is far beyond what is currently known.
Clinical considerations
Always consult a qualified Naturopath for proper assessment and support. For mould/mycotoxin-related conditions, supporting the following may be beneficial:
- Chronic inflammation
- Immune dysregulation
- Gastro-intestinal function and gut barrier integrity
- Supporting clearance of toxins
- Reducing exposure and identifying risk factors
Identifying the sources and causes of mould growth in order to reduce exposure to mould is imperative to promote recovery. The main factor for mitigating mould growth in the indoor environment is by reducing liquid moisture infiltration and moisture as vapour. Understanding the many causes of excess moisture and preventing these risks from occurring in the first place is key to mitigating the risk of future exposure to mould, dampness and mould-related indoor contaminants.22Potential risk factors for sources of indoor mould:18
- Design or construction flaws and inadequate maintenance – leading to water damage
- Natural events such as floods and storms and lack of remediation from damages
- Occupant behaviour which results in flooding of sinks, showers or baths
- Poor ventilation, especially in bathrooms and kitchens
- Behavioural, structural or environmental factors which limit opening of doors and windows.
According to the World Health Organisation, indicators of dampness and microbial growth include the presence of condensation on surfaces or in structures, visible mould, perceived mould odour and a history of water damage, leakage or penetration.106 A thorough inspection, and if necessary, appropriate measuring equipment can be used to determine the presence of indoor moisture and microbial growth.106
Mould can be visible, but can also go undetected. If patients are experiencing multisystem and multi-symptom presentations similar to the biotoxin-related illnesses discussed, further investigation into indoor environments could be warranted.
References
- Kraft, S., Buchenauer, L., & Polte, T. (2021). Mold, Mycotoxins and a Dysregulated Immune System: A Combination of Concern?. International Journal of Molecular Sciences, 22(22), 12269.
- D’Mello, J. F. (1997). Handbook of plant and fungal toxicants. CRC press.
- Janik, E., Niemcewicz, M., Ceremuga, M., Stela, M., Saluk-Bijak, J., Siadkowski, A., & Bijak, M. (2020). Molecular aspects of mycotoxins—A serious problem for human health. International Journal of Molecular Sciences, 21(21), 8187.
- Robbins, C. A., Swenson, L. J., Nealley, M. L., Kelman, B. J., & Gots, R. E. (2000). Health effects of mycotoxins in indoor air: a critical review. Applied occupational and environmental hygiene, 15(10), 773-784.
- Benedict, K., Chiller, T. M., & Mody, R. K. (2016). Invasive fungal infections acquired from contaminated food or nutritional supplements: a review of the literature. Foodborne pathogens and disease, 13(7), 343-349.
- Köhler, J. R., Hube, B., Puccia, R., Casadevall, A., & Perfect, J. R. (2017). Fungi that infect humans. Microbiology spectrum, 5(3), 5-3.
- WHO Mycotoxins. Available online: https://www.who.int/news-room/fact-sheets/detail/mycotoxins
- Lessard, M., Savard, C., Deschene, K., Lauzon, K., Pinilla, V. A., Gagnon, C. A., & Chorfi, Y. (2015). Impact of deoxynivalenol (DON) contaminated feed on intestinal integrity and immune response in swine. Food and Chemical Toxicology, 80, 7-16.
- Gonkowski, S., Gajęcka, M., & Makowska, K. (2020). Mycotoxins and the enteric nervous system. Toxins, 12(7), 461.
- Empting, L. D. (2009). Neurologic and neuropsychiatric syndrome features of mold and mycotoxin exposure. Toxicology and Industrial Health, 25(9-10), 577-581.
- French, P. W., Ludowyke, R., & Guillemin, G. J. (2019). Fungal neurotoxins and sporadic amyotrophic lateral sclerosis. Neurotoxicity Research, 35(4), 969-980.
- Chang, C., & Gershwin, M. E. (2019). The myth of mycotoxins and mold injury. Clinical reviews in allergy & immunology, 57(3), 449-455.
- Rudert, A., & Portnoy, J. (2017). Mold allergy: is it real and what do we do about it?. Expert Review of Clinical Immunology, 13(8), 823-835.
- Nag, P. K. (2019). Sick building syndrome and other building-related illnesses. In Office Buildings (pp. 53-103). Springer, Singapore.
- Köhler, J. R., Casadevall, A., & Perfect, J. (2015). The spectrum of fungi that infects humans. Cold Spring Harbor perspectives in medicine, 5(1), a019273.
- Rosenblum Lichtenstein, J. H., Hsu, Y. H., Gavin, I. M., Donaghey, T. C., Molina, R. M., Thompson, K. J., & Brain, J. D. (2015). Environmental mold and mycotoxin exposures elicit specific cytokine and chemokine responses. PloS one, 10(5), e0126926.
- Shoemaker, R. C., House, D., & Ryan, J. C. (2014). Structural brain abnormalities in patients with inflammatory illness acquired following exposure to water-damaged buildings: a volumetric MRI study using NeuroQuant®. Neurotoxicology and teratology, 45, 18-26.
- Zimmerman, T. (2018). Chronic Inflammatory Immune Response Syndrome (CIRS). Inquiry into Bio-toxin related illness. Parliament of Australia. https://www.aph.gov.au
- Shoemaker, R.C., Johnson, K., Lysander, J., Berry, Y., Dooley, M., Ryan, J. & McMahon, S. (2018). Diagnostic process for chronic inflammatory response syndrome (CIRS): A consensus statement report of the consensus committee of surviving mold. Internal medicine review, (6)
- Shoemaker, R. C., & House, D. E. (2006). Sick building syndrome (SBS) and exposure to water-damaged buildings: time series study, clinical trial and mechanisms. Neurotoxicology and teratology, 28(5), 573-588.
- Kenneth W. Umbach, Pamela J. Davis, Indoor Mold A General Guide to Health Effects, Prevention, and Remediation, California Research Board Report in Response to A.B. 284, Chapter 550, Statutes of 2001, 2006
- Coulburn, L., & Miller, W. (2022). Prevalence, Risk Factors and Impacts Related to Mould-Affected Housing: An Australian Integrative Review. International Journal of Environmental Research and Public Health, 19(3), 1854.
- Vaillant, A. A. J., Vashisht, R., & Zito, P. M. (2021). Immediate Hypersensitivity Reactions. In StatPearls [Internet]. StatPearls Publishing.
- Hedayati, M. T., Pasqualotto, A. C., Warn, P. A., Bowyer, P., & Denning, D. W. (2007). Aspergillus flavus: human pathogen, allergen and mycotoxin producer. Microbiology, 153(6), 1677-1692.
- Bowyer, P., Fraczek, M., & Denning, D. W. (2006). Comparative genomics of fungal allergens and epitopes shows widespread distribution of closely related allergen and epitope orthologues. BMC genomics, 7(1), 1-14.
- Twaroch, T. E., Curin, M., Valenta, R., & Swoboda, I. (2015). Mold allergens in respiratory allergy: from structure to therapy. Allergy, asthma & immunology research, 7(3), 205-220.
- Mims, J. W. (2015, September). Asthma: definitions and pathophysiology. In International forum of allergy & rhinology (Vol. 5, No. S1, pp. S2-S6).
- Vincent, M., Percier, P., De Prins, S., Huygen, K., Potemberg, G., Muraille, E., & Denis, O. (2017). Investigation of inflammatory and allergic responses to common mold species: Results from in vitro experiments, from a mouse model of asthma, and from a group of asthmatic patients. Indoor Air, 27(5), 933-945.
- Dykewicz, M. S., Rodrigues, J. M., & Slavin, R. G. (2018). Allergic fungal rhinosinusitis. Journal of Allergy and Clinical Immunology, 142(2), 341-351.
- Møller, J., Hyldgaard, C., Kronborg-White, S. B., Rasmussen, F., & Bendstrup, E. (2017). Hypersensitivity pneumonitis among wind musicians–an overlooked disease?. European clinical respiratory journal, 4(1), 1351268.
- Sakamoto, T., Yamasaki, A., Funaki, Y., Harada, T., Okazaki, R., Hasegawa, Y., & Shimizu, E. (2018). An onion farmer with a case of hypersensitivity pneumonitis caused by Aspergillus niger. Respiratory medicine case reports, 23, 60-62.
- Mohr, L. C. (2004). Hypersensitivity pneumonitis. Current opinion in pulmonary medicine, 10(5), 401-411.
- Benkerroum, N. (2020). Chronic and acute toxicities of aflatoxins: Mechanisms of action. International journal of environmental research and public health, 17(2), 423.
- Shirani, K., Zanjani, B. R., Mahmoudi, M., Jafarian, A. H., Hassani, F. V., Giesy, J. P., & Karimi, G. (2018). Immunotoxicity of aflatoxin M1: as a potent suppressor of innate and acquired immune systems in a subacute study. Journal of the Science of Food and Agriculture, 98(15), 5884-5892.
- Reif, D. M., Martin, M. T., Tan, S. W., Houck, K. A., Judson, R. S., Richard, A. M., & Kavlock, R. J. (2010). Endocrine profiling and prioritization of environmental chemicals using ToxCast data. Environmental health perspectives, 118(12), 1714-1720.