Have you moved your bowels today? If so, how was it? These are not common questions asked outside a naturopathic clinic and many people I ask similar questions of are quite vague in their responses. Many say they don’t look. Bowel motions reflect the overall health of your digestive system so it pays to be more aware of what you leave behind in the loo.
Chronic idiopathic constipation (CIC) is one of the most common functional gastrointestinal disorders worldwide, with a global prevalence of 14%. One in four Australians (over 6 million) people are affected by constipation. It is more common in women and its prevalence increases with age, significantly impacting quality of life. People experiencing CIC usually present with symptoms such as hard or lumpy stools, reduced frequency of defecation, a sensation of incomplete evacuation or blockage, straining, abdominal pain and bloating.
A multifaceted approach is required for the management of CIC which addresses all potential contributing factors. Lifestyle modifcations, such as increasing dietary fibre, hydration and exercise are usually the first steps in managing CIC. In addition, the management of constipation can be supported with specific evidence-based herbal medicines. There are a few key herbs that provide effective laxative support, whilst also addressing many of the driving factors of constipation. [Speak to your naturopath or herbalist]
Herbs and other supplements may help to alleviate constipation by increasing lower gut motility and bile flow, whilst providing soothing muco-protective actions for lower gut integrity and mucous membranes.
Constipation affects 1 in 4 Australians, the most common being functional constipation
Functional constipation is usually caused by one or a combination of the following: dehydration, sedentary lifestyle, gut microbiota dysbiosis, food sensitivity/intolerance, stress, psychological factors, inadequate dietary fibre and/or fluid intake, small intestinal bacterial overgrowth (SIBO), IBS, anal fissures, and some medications, such as opiates or tricyclic anti-depressants.
Additionally, constipation can be secondary to neurological conditions, such as Parkinson’s disease and multiple sclerosis, endocrine disorders such as hypothyroidism and hypercalcaemia, structural disorders (strictures, rectoceles, colon cancer), and myopathic diseases (scleroderma, myotonic dystrophy). Although coeliac disease is more commonly associated with diarrhoea, a large cohort study has shown coeliac disease is associated with constipation in 10% of patients. Obstetric and gynaecological history should also be considered in women suffering constipation or any bowel disorders.
Pathophysiology of Constipation
Although the pathophysiology remains unclear, research suggests alterations in the colonic microbiota can increase bile acid metabolism, promote methane production, and affect epithelial function, all of which can alter colonic motility and fluid secretion, resulting in constipation. A recent study found constipation to cause a significant reduction in the production of short chain fatty acids (SCFAs) and a higher level of iso-butyrate. Stool samples from constipated patients showed a reduced abundance of specific lactate and butyrate-producing microbiota, Faecalibacterium, Ruminococcaceae and Roseburia, and elevated endotoxin producing bacteria Desulfovibrionaceae.
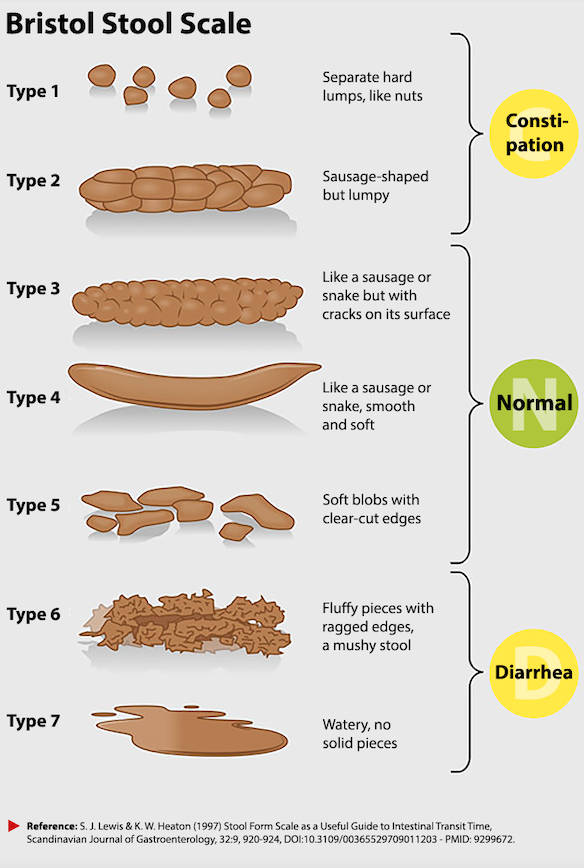
If you have been experiencing CIC, or other bowel-related discomfort, it may be worth discussing functional testing with your naturopath. A comprehensive stool and parasitology analysis helps identify imbalanced microbiome and presence of unwanted microbes. If you are unsure, check the Bristol Stool Chart below.
What you can do
- Ensure you are drinking enough fluids, preferably purified water and/or herbal tea. Avoid caffeinated drinks like coffee, tea and green tea as these can exacerbate fluid loss.
- Increase fresh vegetable* and fruit* intake – aim to eat 600 grams of non-starchy vegetables and fruit daily.
- Increase fibre* intake – oats, barley, quinoa, sweet corn, brown rice, beans, lentils, chic peas
- Ensure your stomach acid levels are adequate to get the digestive process started. Low stomach acid can be due to stress or medication, especially ant-acids or proton-pump inhibitors.
- Avoid snacking constantly to give your bowels a chance to empty and ‘self-clean’ in between meals
- Go for a walk. Walking is an underestimated yet important form of daily exercise. Park your car at the far end of the parking area and walk to the shops, or use stairs instead of the lift of escalator.
* always select organic or unsprayed produce whenever possible as chemicals used in commercial agriculture have been shown to disrupt healthy gut function
Always seek the advice of a qualified natural health practitioner and don’t self-prescribe.

