At its worst, anxiety can be debilitating, affecting people physically and mentally and stopping them from living their best lives. This year has been a particularly challenging year for many, facing bushfires and the considerable impacts on daily life due to coronavirus (COVID-19). Anxiety exists in all corners of the country: city and rural, and in men, women, and children. Research indicates approximately 25% of adult Australians have above normal levels of anxiety symptoms1, however in the current COVID-19 climate, many more will be feeling anxious.
Rumination over everyday life factors including work and family issues, financial stress and illness can spiral out of control, leading to anxiety, difficulty sleeping, or both. In addition, long term stress/anxiety can lead to a number of physical, psychological and behavioural imbalances:

At True Medicine we are able to support your needs with targeted treatments that help calm anxiety and restore healthy sleep patterns. Furthermore, we provide a holistic approach which includes education on healthy eating, exercise and lifestyle modifications to help you maintain optimal health well into the future.
Here’s the science on how herbal remedies can support anxiety and mood imbalances.
The Balance Between Neurotoxicity and Neuroprotection
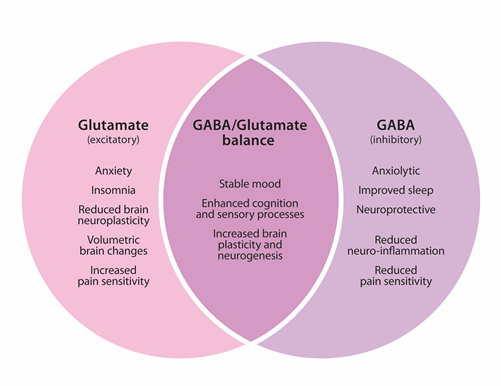
Anxiety, as with other mood imbalances, can represent underlying hypothalamic-pituitary-adrenal (HPA) axis dysfunction and may be underpinned by an imbalance between neurotoxic and neuroprotective factors, as seen mirrored in the opposing relationship between glutamate and gamma-aminobutyric acid (GABA) (see Figure 1). These related neurotransmitters create opposing inhibitory and excitatory effects, and constitute the vast majority of all neurotransmission in the brain.2 They are the primary neurotransmitters of concern in anxiety and also play a major role in sleep disorders. Excessive glutamate is a prime example of a neurotoxic factor, which personifies generalised anxiety disorder. This may be seen clinically as restlessness, nervous tension, anxiety and difficulty sleeping, which over the long term may lead to reduced neuroplasticity. This is in contrast to the neuroprotective and inhibitory GABA, which promotes a sense of calm, supports healthy sleep, and reduces stress induced inflammation.3
Chronic stress may result in changes to the structure and function of particular brain regions (e.g. the hippocampus and prefrontal cortex); the HPA axis which mediates the stress response, bears this brunt. The resulting impact may have deleterious effects for neuronal, metabolic, endocrine and immune systems.4 This is best illustrated by what occurs in the hippocampus: when cortisol binds to glucocorticoid receptors there, it stimulates the release of glutamate. An appropriate level of glutamate is necessary for memory and learning, however excessive glutamate is toxic, leading to neuronal dendritic retraction and under functioning and shrinkage of the hippocampus.5 These alterations are strongly associated with mood disorders, including anxiety and panic disorder.6 Therefore, chronic anxiety and/or poor sleep can have significant consequences for patients both now and in the future.
Neuroprotective Factors and Helpful Herbs
Fortunately, offsetting neurotoxicity and promoting beneficial neuroplasticity is possible. Supporting GABA production helps reverse the effects of glutamate and enhances healthy sleep. This is the primary mechanism of anxiolytic medications such as benzodiazepines. Whilst meditation and yoga increase GABA directly,7 and exercise has the ability to modulate both GABA and glutamate8, certain herbal medicines may also modulate these neurotransmitters. Traditionally used to manage mental stress, current research is now substantiating the use of herbs, showing anxiolytic and sedative actions comparable to those seen in pharmaceutical medications.9,10,11
Herbal Support to Calm the Anxious Mind
Providing much-needed relief are herbs that can help alleviate symptoms of anxiety and nervous tension. Some herbs used have a long history in traditional Chinese medicine (TCM) for the treatment of anxiety and related conditions.12 These herbs are rich in active compounds which protect against neuronal cell damage and promote central inhibitory activity.13 The jujuboside compound has the ability to inhibit glutamate’s excitatory activity on hippocampal neurons, decreasing excessive excitation and promoting anxiolytic-like effects.14,15 Other herbs also contain biologically active compounds with neuroprotective properties which inhibit glutamate and N-methyl-D-aspartate receptor (NMDA) activation, promote healthy neuronal connectivity, support healthy brain plasticity, and also aid muscle relaxation.16,17,18,19 The affinity of some herbs for the GABA benzodiazepine receptor was shown to be strong,20 supporting anxiolytic actions.
TCM herbs are used for their anxiolytic effects, with the constituents demonstrating beta-adrenoceptor blocking activity,21,22 supporting a sense of calm. A double-blind, crossover trial compared a herb used in natural medicine (260 mg/d) with the benzodiazepine midazolam in 40 patients to mitigate anxiety experienced prior to dental surgery. The patients received either the herb or midazolam 30 minutes prior to surgery, and anxiety was assessed at the initial consultation, and before each of the two surgical procedures. Analysis found no statistical differences between herb and the pharmaceutical at any stage, indicating a comparable anxiolytic effect.23 Current research exemplifies how these select herbal extracts are highly effective in mitigating anxiety in patients, helping to restore normal daily functioning.
Herbs for a Better Night’s Sleep
Not surprisingly, some of the same herbs can also promote healthy sleep. The extracts found in these herbs which have been used traditionally for generations, and now scientific evidence is backing up these claims. The herb “P” was trialled on 154 subjects experiencing insomnia and nervous tension for 12 weeks, using on average 1,020 mg/d of dried extract. Results achieved an improvement in sleep disturbances, indicating positive effects on sleep maintenance and quality, as well as reductions in restlessness and nervous tension.24 Research has also noted that herbal extracts do not impair memory or motor skills,25,26 and lack the potential for dependence unlike that associated with benzodiazepines;27 making these a safer option for long-term use.
Some pure essential oils have also been shown to mitigate anxiety and insomnia through GABAergic properties; these effects have been compared to the GABA analogue, pregabalin.28 A double-blind, placebo-controlled 10 week trial aimed to analyse the relaxing effects of a specific essential oil in a group of 170 patients. In all outcome measures including anxiety and sleep quality, the effect of the essential oil surpassed that of the placebo, with the researchers concluding that essential oils produced beneficial effects in patients suffering with anxiety and poor sleep.29 Further studies using herbs demonstrated sedative effects via endogenous alkaloids, with certain constituents acting as weak stimulators of the GABAA receptor30,31; used traditionally for its sleep promoting but also pain-relieving properties.32 Other herbs were shown to provide analgesic relief and having a long history of use for neuralgic pain.33,34,35 Herbs exhibit an antispasmodic effect to suppress spasm of smooth muscle,36 highlighting the use of their for the treatment of pain, muscular spasm and nervous tension. Studies confirmed that specific herbs used together help patients get a good night’s sleep, particularly when nervous tension and/or pain are compromising sleep quality.
Helping you live your best life
Carefully selected herbal medicines can have positive GABAergic and neuroprotective effects to help you overcome symptoms of anxiety and disturbed sleep; however a truly holistic approach will also include nutritional interventions and dietary and lifestyle strategies that provide a solid foundation for long-lasting improvements. At True Medicine we provide a holistic approach which includes education on healthy eating, exercise and lifestyle modifications. This approach may provide a strong foundation for you to move beyond debilitating anxiety or insomnia and enable you to live your best life.
Call the clinic on 07 5530 1863 for an appointment. On-line consultations are now available.
References:
1 Australian Psychological Society. Stress & wellbeing: how Australians are coping with life [Internet]. Melbourne: Australian Psychological Society, 2015. [cited 2020 Jan 1]. Available from: https://www.psychology.org.au/getmedia/ae32e645-a4f0-4f7c-b3ce-dfd83237c281/stress-wellbeing-survey.pdf.
2 Wierońska JM, Stachowicz K, Nowak G, Pilc A. The loss of glutamate-GABA harmony in anxiety disorders. Edited by Vladimir V. Kalinin. 2011 Aug 1:135.
3 Crowley T, Cryan JF, Downer EJ, et al. Inhibiting neuroinflammation: The role and therapeutic potential of GABA in neuro-immune interactions. Brain Behav Immun. 2016;54:260-277.
4 Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol. 2005;67:259-284.
5 Stein-Behrens BA, Lin WJ, Sapolsky RM. Physiological elevations of glucocorticoids potentiate glutamate accumulation in the hippocampus. J Neurochem. 1994 Aug;63(2):596-602.
6 Meyerhoff DJ, Mon A, Metzler T, Neylan TC. Cortical gamma-aminobutyric acid and glutamate in posttraumatic stress disorder and their relationships to self-reported sleep quality. Sleep. 2014 May 1;37(5):893-900. doi:10.5665/sleep.3654.
7 Streeter CC, Jensen JE, Perlmutter RM, Cabral HJ, Tian H, Terhune DB, et al. Yoga asana sessions increase brain GABA levels: a pilot study. J Altern Complement Med. 2007 May 1;13(4):419-26.
8 Maddock RJ, Casazza GA, Fernandez DH, Maddock MI. Acute modulation of cortical glutamate and GABA content by physical activity. J Neurosci. 2016 Feb 24;36(8):2449-57.
9 Akhondzadeh S, Naghavi HR, Vazirian M, Shayeganpour A, Rashidi H, Khani M. Passionflower in the treatment of generalized anxiety: A pilot double‐blind randomized controlled trial with oxazepam. J Clin Pharm Ther. 2001 Oct 30;26(5):363-7.
10 Woelk H, Schläfke S. A multi-center, double-blind, randomised study of the Lavender oil preparation Silexan in comparison to Lorazepam for generalized anxiety disorder. Phytomedicine. 2010 Feb 1;17(2):94-9.
11 Seo JJ, Lee SH, Lee YS, Kwon BM, Ma Y, Hwang BY, et al. Anxiolytic-like effects of obovatol isolated from Magnolia obovata: involvement of GABA/benzodiazepine receptors complex. Prog Neuropsychopharmacol. 2007 Oct 1;31(7):1363-9.
12 Chen CJ, Li M, Wang XL, Fang FF, Ling CQ. Effect of Sour Date (Semen ziziphi spinossae) seed extract on treating insomnia and anxiety. In: Nuts and Seeds in Health and Disease Prevention. London, Academic Press. 2011. p. 1037-1041.
13 Han H, Ma Y, Eun JS et al. Anxiolytic-like effects of sanjoinine A isolated from Zizyphi Spinosi Semen: possible involvement of GABAergic transmission. Pharmacol Biochem Be. 2009;92(2):206-213.
14 Zhang M, Ning G, Shou C, Lu Y, Hong D, Zheng X. Inhibitory effect of jujuboside A on glutamate-mediated excitatory signal pathway in hippocampus. Planta Med. 2003;69(8):692-695.
15 Han H, Ma Y, Eun JS, Li R, Hong JT, Lee MK, et al. Anxiolytic-like effects of sanjoinine A isolated from Zizyphi Spinosi Semen: possible involvement of GABAergic transmission. Pharmacol Biochem Be. 2009;92(2):206-213.
16 Woodbury A, Yu SP, Wei L, García P. Neuro-modulating effects of honokiol: a review. Front Neurol. 2013:4(130);2-4. doi: 10.3389/fneur.2013.00130
17 Lee YJ, Lee YM, Lee CK, Jung JK, Han SB, Hong JT. Therapeutic applications of compounds in the Magnolia family. Pharmacol Ther. 2011;130(2):157-176.
18 Han H, Ma Y, Eun JS, Li R, Hong JT, Lee MK, et al. Anxiolytic-like effects of 4-O-Methylhonokiol isolated from Magnolia officinalis through enhancement of GABAergic transmission and chloride influx. J Med Food. 2011;14(7):724 -731.
19 Woodbury A, Yu SP, Wei L, García P. Neuro-modulating effects of honokiol: a review. Front Neurol. 2013:4(130);2-4. doi: 10.3389/fneur.2013.00130.
20 Koetter U, Barrett M, Lacher S, Abdelrahman A, Dolnick D. Interactions of Magnolia and Ziziphus extracts with selected central nervous system receptors. J Ethnopharmacol. 2009;124(3):421-425.
21 Wang LY, Zhao AP, Chai XS. Effects of puerarin on cat vascular smooth muscle in vitro. Acta Pharmacologica Sinica. 1994;15(2):180-182.
>22 Wong KH, Li GQ, Li KM, Razmovski-Naumovski V, Chan K. Kudzu root: traditional uses and potential medicinal benefits in diabetes and cardiovascular diseases. J Ethnopharmacol. 2011;134(3):584-607.
23 Dantas LP, Oliveira Ribeiro A, Almeida-Souza LM, Groppo FC. Effects of passiflora incarnate and midazolam for control of anxiety in patients undergoing dental extraction. Med Oral Patol Oral Cir Bucal. 2017 Jan 1;22(1):95-10. doi: http://dx.doi.org/doi:10.4317/medoral.21140
24 Gibbert J, Kreimendahl F, Lebert J, Rychlik R, Trompetter I. Improvement of stress resistance and quality of life of adults with nervous restlessness after treatment with a passionflower dry extract. Complement Med Res. 2017April 12;24:83-89. doi:10.1159/000464342.
25 Passion flower. In: Natural Medicines Comprehensive Database [database on the Internet]. Stockton (CA): Therapeutic Research Faculty; 1995-2008 [cited 2017 Feb 13]. Available from: http://www.naturaldatabase.com. subscription required to view.
26 Akhondzadeh S, Naghavi HR, Vazirian M, Shayeganpour A, Rashidi H, Khani M. Passion flower in the treatment of generalized anxiety: a pilot double-blind randomized controlled trial with oxazepam. J Clin Pharm Ther. 2001;26(5):363-7.
27 Dhawan K, Dhawan S, Chhabra S. Attenuation of benzodiazepine dependence in mice by a tri-substituted benzoflavone moiety of Passiflora incarnata Linneaus: a non-habit forming anxiolytic. J Pharm Pharm Sci. 2003;6(2):215-22.
28 Kasper S, Anghelescu I, Dienel A. Efficacy or orally administered Silexan in patients with anxiety-related restlessness and disturbed sleep- a randomized, placebo-controlled trial. Eur Neuropsychopharmacol. 2015 July 28;25:1960-67. doi:http://dx.doi.org/10.1016/j.euroneuro.2015.07.024
29 Kasper S, Anghelescu I, Dienel A. Efficacy or orally administered Silexan in patients with anxiety-related restlessness and disturbed sleep- a randomized, placebo-controlled trial. Eur Neuropsychopharmacol. 2015 July 28;25:1960-67. doi:http://dx.doi.org/10.1016/j.euroneuro.2015.07.024
30 Fedurco M, Gregorova J, Sebrlova K, Kantorova J, Pes O, Baur R, et al. Modulatory effects of Eschscholzia californica alkaloids on recombinant GABAA receptors. Biochem Res Int. 2015 Sept 15; 2015:617-620. doi:http://dx.doi.org/10.1155/2015/617620.
31 Rolland A, Fleurentin J, Lanhers MC, Misslin R, Mortier F. Neurophysiological effects of an extract of Eschscholzia californica Cham.(Papaveraceae). Phytother Res. 2001 Aug;15(5):377-81.
32 Bone, K. A Clinical Guide to Blending Liquid Herbs. Warwick, Queensland; Churchill Livingstone; 2003. p. 206-209.
33 Ellingwood F. Piscidia erythrina. The American materia medica, therapeutics and pharmacognosy. [Internet]. Chicago (IL): 1919 [cited 2018 Sept 18]. Available from: https://www.henriettes-herb.com/eclectic/ellingwood/piscidia.html.
34 Felter HW. Piscidia. The eclectic materia medica, pharmacology and therapeutics. [Internet]. Cincinnati (OH): 1922 [cited 2018 Sep 18]. Available from: https://www.henriettes-herb.com/eclectic/felter/piscidia.html.
35 Felter HW, Lloyd JU. Piscidia.-Jamaica Dogwood. King’s American Dispensatory. 18th ed. 3rd Revision. [Internet]. Cincinnati (OH): Ohio Valley Co.; 1898. [cited 2018 Sep 18]. Available from: https://www.henriettes-herb.com/eclectic/kings/piscidia.html.
36 Bone K. A clinical guide to blending liquid herbs: herbal formulations for the individual patient. St Louis (MO): Elsevier/Churchill Livingstone; 2003. p. 289-290.

