Science and research are ongoing, often revealing new evidence that sometimes challenges long-standing and long-held theories. What precedes many of these scientific findings is decades of clinical evidence – so once science catches up, it’s really exciting.
SHATTERING THE SEROTONIN THEORY OF DEPRESSION
“Although it is often stated with great confidence that depressed people have a serotonin or norepinephrine deficiency, the evidence actually contradicts these claims” Professor Emeritus of Neuroscience Elliot Valenstein.
The ‘neurotransmitter imbalance’ model of depression was first hypothesised in the mid-1960s and has since been popularised by pharmaceutical companies, educators, medical practitioners, and the media. The belief that anxiety and depression are caused by a serotonin deficit at the synaptic cleft has led to widespread prescription and use of anti-depressant medications targeting serotonin reuptake (selective serotonin reuptake inhibitors or SSRIs). Anti-depressant medications have become the most frequently prescribed medications for mental disorders worldwide and among the top ten most prescribed medications in Australia. The validity of the serotonin imbalance supposition has been called into question, with a 2022 umbrella review by Moncrieff et al revealing very little evidence to support the theory. Umbrella reviews examine available meta-analyses and clinical studies to form one of the highest levels of evidence currently available.
Research fails to validate the neurotransmitter imbalance model
If the serotonin hypothesis were accurate, then the mechanisms by which serotonin becomes depleted should, in theory, be affected in depressed and anxious patients. When examining the various mechanisms involved in serotonin deficit, Moncrieff at al reviewed serotonin and its metabolites in blood and cerebrospinal fluid and found no significant differences between depressed patients and controls. Similarly, dietary restriction of tryptophan and the resulting depletion of serotonin did not induce depression in most studies (minor effects were found in one small study only). Likewise, examination of the receptors, transporters and genes involved in serotonin reuptake and recycling yields no convincing evidence in support of the serotonin depletion theory.
A holistic approach to mental disorders
With this in mind, and the fact that anti-depressant medication works adequately for approximately just one third of users, it is worth considering that the aetiology of mental health disorders extends beyond a simple neurotransmitter imbalance and is better conceptualised within a holistic framework.
Recent research points to the notion that mental health disorders such as anxiety and depression are the result of an interaction between various body systems, illuminating multiple opportunities for therapeutic intervention.
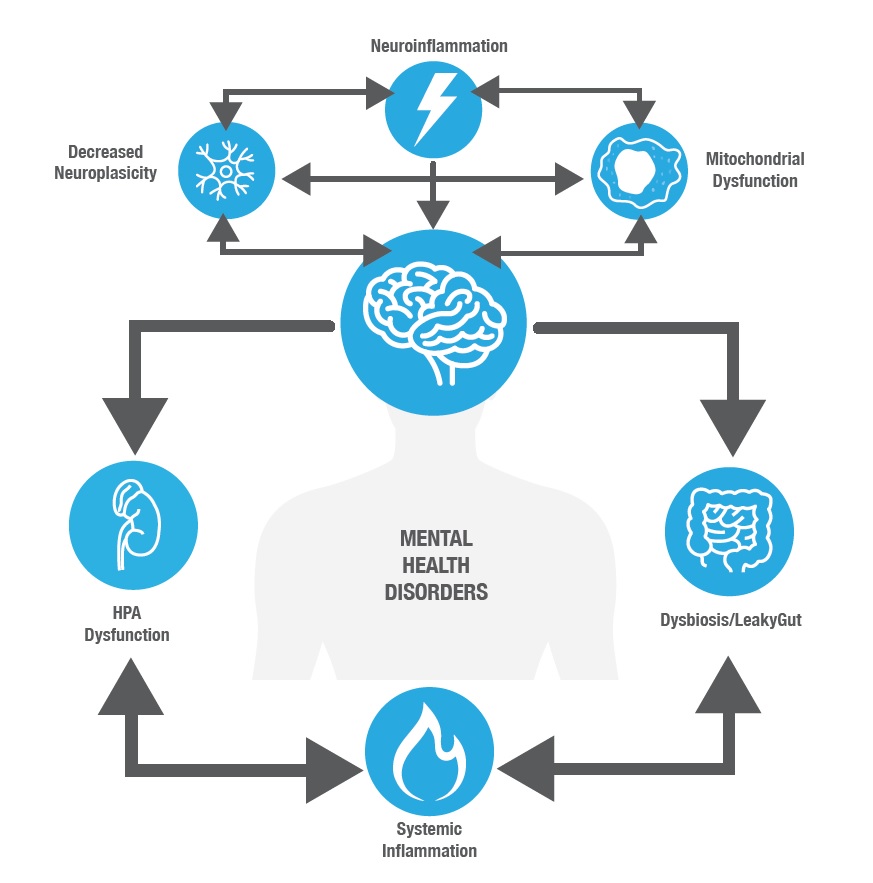
Current evidence points towards three key underlying imbalances that precede, and perpetuate the vicious cycle driving neurological dysfunction (See Figure 1):
1. Chronic stress and hypothalamic-pituitary-adrenal (HPA) axis dysfunction
2. Systemic and neuro-inflammation
3. Gut dysfunction
Each imbalance drives the other, and contributes to mitochondrial dysfunction in the brain and reduced neuroplasticity; both of which underpin many mental health and neurological conditions.
Figure 1. Contributors to the underlying dysfunctions involved in mental health disorders
Stress, inflammation and gut dysfunction as drivers
STRESS AND HPA DYSFUNCTION
Chronic stress and HPA dysfunction are considered underlying and predisposing factors in the development of anxiety, depression and phobias, disrupting mitochondrial function and neuroplasticity. Acute and chronic stress further contribute to mental disorders by inducing systemic inflammation and disrupting gut function. Alterations in intestinal permeability (IP) and microbial balance, increase neuro-inflammation, compounding the effects of stress on neuroplasticity and mitochondrial dysfunction.
SYSTEMIC AND NEURO-INFLAMMATION
Systemic inflammation is known to be present in a large number of psychiatric disorders and can precede depressive events, suggesting a causative mechanism. Like stress, systemic inflammation is associated with neuro-inflammation, which drives the mitochondrial dysfunction and reduced neuroplasticity present in many mental health disorders.
DYSBIOSIS AND GUT HEALTH
Complex bi-directional communication between the gut and the brain means that the health of one system relies heavily on the health of the other. Dysbiosis and IP not only promote systemic and neuro-inflammation, but also directly affect the central nervous system and mental health disorders. Peptide hormones and short chain fatty acids released from the gut, efferent vagus nerve transmission and immune system communications facilitate information transfer from the gut to the brain. Specific probiotic strains which optimise gut health and reduce systemic inflammation may also aid the management of mood disorders.
Conclusion
With new understanding of the pathophysiological mechanisms underlying mood disorders comes new opportunities for intervention.
Emerging research guides the practitioner towards a holistic and foundational approach to mental health and once again returns our focus to the gut: the seat of all health.
For more information or to listen to the psychiatrists: https://theconversation.com/depression-is-probably-not-caused-by-a-chemical-imbalance-in-the-brain-new-study-186672?hss_channel=fbp-479163965435700