Oral microbial health can influence the health of teeth and gums, as well as systemic health.
As we are beginning to understand, the body contains may distinct microbiomes. The oral cavity is no exception, harbouring up to 200 microbial species per person and several discrete microbial colonies on the different surfaces available for adherence (teeth, gums, tongue, cheeks, lips and the palates). As with any microbial colony, the diversity and health of the oral microbiome can
vary significantly in different patients, influencing not only oral health but also systemic health.
What does a healthy oral microbiome look like?
There is currently no accurate model of a healthy oral microbiome, however research indicates that oral dysbiosis is characterised by:
a) The presence of virulent and/or opportunistic pathogens such as Streptococcus mutans, Porphyromonas gingivalis and Treponema denticola; and/or
b) A loss of microbial diversity within the mouth.
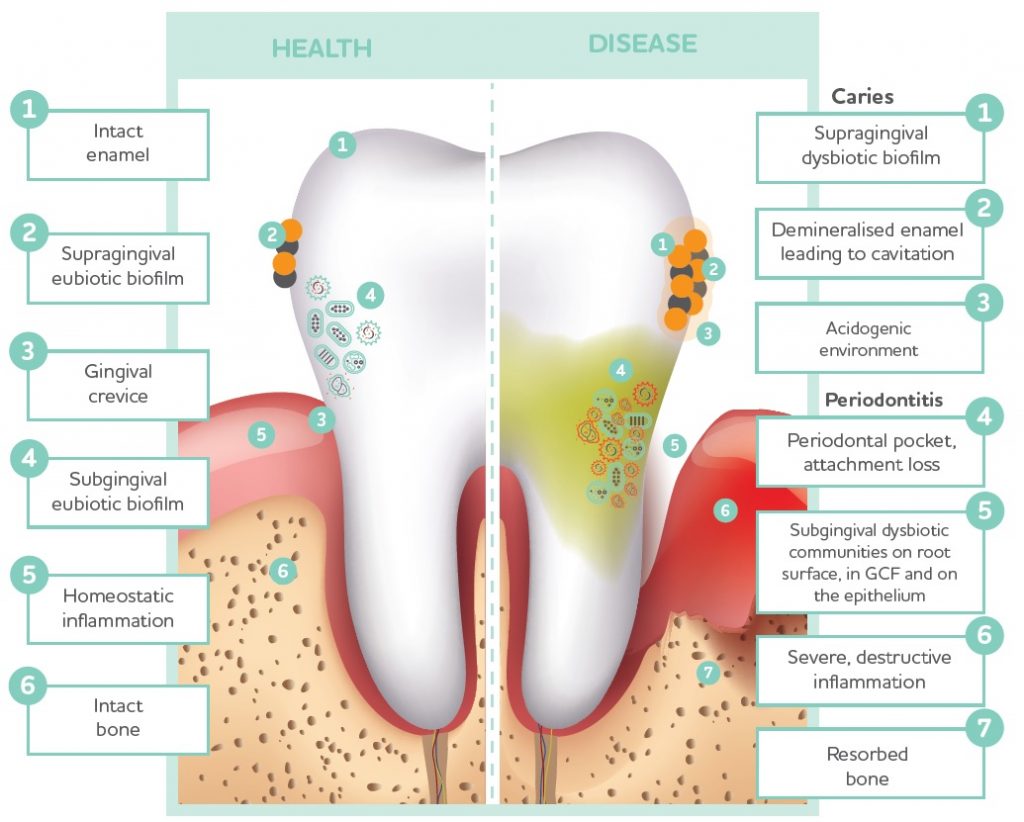
Healthy teeth and gums linked to oral microbiome
The health of the mouth, teeth, and gums is particularly influenced by the health and diversity of the oral microbiome. A complex interplay between the oral microbiota, carbohydrate availability, and pH balance all contribute to the development of dental caries,
gingivitis and periodontitis.
What drives oral dysbiosis?
The development of dental caries, gingivitis and periodontitis is characterised by a shift towards a pathogenic oral microbiome profile. This process relies on several factors including:
- Dietary sugars – High consumption to sugar is known to drive oral dysbiosis as sugars provide a substrate for the pathogenic bacteria to feed on and proliferate.
- Acid/base balance – A healthy oral microbiome exists in a pH range from 5.5-7.0. An acidogenic shift can occur due to prolonged exposure to excess carbohydrates allowing the proliferation of cariogenic bacteria. Systemic pH is the main determinant of salivary pH, though consumption of acidic foods (e.g. wine, soft drinks) also contributes to oral acidity.
Once again, pH becomes so very important in optimal functioning throughout the body.
Saliva production – Salvia regulates the microbiome through production of immunoglobulins and flushes away carbohydrates from food that microbes would otherwise feed on. It also removes acids from food and carbohydrate fermentation that can promote further dysbiosis and dental enamel erosion. Inadequate saliva production promotes plaque formation.
Dental plaque – This is a combination of microbes and biofilm and although not in itself an indicator of dysbiosis, it is necessary for tooth decay and periodontitis. Regular removal of plaque with a toothbrush and interdental device (floss or interdental brushes) alongside professional tooth cleaning is recommended.
Lifestyle factors – Key factors such as cigarette smoking, dehydration, and stress can impair oral health through their impact on salivary pH, microbial balance, localised inflammation, and oral levels of oxidative stress.
Sugar consumption is a key driver of oral dysbiosis – there is effectively a feedforward loop where refined carbohydrate intake and dysbiosis leads to acidification of the plaque, promoting further dysbiosis, which then leads to destruction of enamel and demineralisation of the tooth.
Systemic effects of oral dysbiosis
Oral dysbiosis not only causes disease within the oral cavity, it is also associated with many systemic diseases including cardiovascular disease, obesity and diabetes, mental health, as well as preterm birth and low birth weight babies. These extra-oral consequences appear to be due to increased inflammatory mediators and/or bacterial translocation, although the exact mechanisms are still being investigated. Maintaining good oral health through diet, dental hygiene practices and supporting the oral microbiome is essential not just for dental and gum health, but for reducing the risk of systemic disease and negative birth outcomes.
Source: BioPractica Health Review

